Arthritis
14th Jan 2021
All you need to know about arthritis
Key points
Arthritis is inflammation of the joints causing pain and reduction of mobility (NHS website). There are two main groups; firstly, ‘wear and tear’ called osteoarthritis (OA) and secondly arthritis associated with an autoimmune disease, such as Rheumatoid arthritis (RA).
In the UK, more than 10 million people suffer with some form of arthritis, with OA being most common. While there are analgesic medications (pain-killers) that can help with the symptoms of arthritis, and disease modifying anti-rheumatic drugs (DMARDs) for RA, is there evidence to support any benefit from lifestyle changes?
Osteoarthritis
With age, there is increased risk of breakdown of the cartilage that protects the end of the bones, leading to pain, swelling and reduced movement. People suffering with OA are at risk of progressive worsening of pain and limitation of movement. Treatment options are very limited and are restricted to pain management only, such as paracetamol and non-steroidal anti-inflammatories like ibuprofen, but they do not alter the progression of the disease. These drugs, while generally safe, do have side-effects associated with them.
Autoimmune arthropathies
There are a number of different autoimmune conditions that are associated with arthritis, but of these Rheumatoid arthritis (RA), is the most common arthritis, and affects nearly 1% of the world’s population. Why RA develops is not clear, but it is thought that genetic factors account for approximately 50-60% of the risk, while lifestyle factors may account for the remainder (Alwarith, Kahleova, Rembert, et al., 2019).
Can diet help osteoarthritis arthritis?
Weight
Excess weight is known to play a role as a risk factor for development of OA, not just through physical application of an increased load, but also from the associated inflammation seen with obesity and associated risk of an abnormal cholesterol profile (Thomas, Browne, Mobasheri, et al., 2018). Weight reduction for overweight patients ideally through a combination of diet and exercise is important (Thomas, Browne, Mobasheri, et al., 2018) and a 5% reduction of weight, in people who were overweight with OA, has been associated with improvement in function and pain (Thomas, Browne, Mobasheri, et al., 2018).
Exercise
Exercise not only helps with weight loss, but also leads to metabolic changes and reduced inflammation (the adipokine profile) (Thomas, Browne, Mobasheri, et al., 2018). Therefore, diet and exercise together are more effective than just dietary changes alone. Exercise that combines strengthening, aerobic exercise and flexibility is most likely to improve pain and function (Uthman, van der Windt, Jordan, et al., 2013). Strengthening exercises and quality protein, can help to maintain muscle mass while reducing fat percentage, which aids mobility with OA (Thomas, Browne, Mobasheri, et al., 2018).
Blood sugar
Raised blood sugar seen in type 2 diabetes, is associated with impaired subchondral bone formation (the area just below the cartilage), and reduced function of the cartilage (Zhuo, Yang, Chen, et al., 2012). Type 2 diabetes has also been identified as a risk factor for severe OA and a predictor for knee/hip replacement (Schett, Kleyer, Perricone, et al., 2013).
Cholesterol
Worsening risk of OA progression has been linked with not just type 2 diabetes, but also metabolic syndrome (the combination of diabetes, abnormal cholesterol profile, high blood pressure and obesity) (Thomas, Browne, Mobasheri, et al., 2018).
Raised cholesterol is associated with type 2 diabetes and metabolic syndrome, both of which are associated with increased risk of OA. A benefit has been seen when cholesterol is lowered by dietary changes or statin medications suggesting abnormal cholesterol is implicated in the mechanism of OA (Thomas, Browne, Mobasheri, et al., 2018).
Fats
A large prospective study in patients with OA found that a higher intake of total and saturated fat was associated with an increased risk of worsening OA; whereas higher intake of unsaturated fats was associated with decreased progression of OA measured via X-rays (Lu, Driban, Xu, et al., 2017). Current opinion is that the metabolic products of omega 3 fatty acids are less inflammatory than those produced from omega 6 fatty acids. Western diets are associated with an imbalance of omega 3/6 such that instead of levels of omega 3 being higher than 6, the reverse is more commonly seen. This is associated with an increased risk of chronic inflammation (Kaliannan, Wang, Li, et al., 2015).
Vitamin K
Vitamin K is an important micronutrient for bone and cartilage health and increasing vitamin K intake may benefit OA (Thomas, Browne, Mobasheri, et al., 2018; Chin, 2020). The term ‘Vitamin K’, can refer to a number of different molecules, and these are found in green vegetables, fermented food, dairy, and meat. You need to eat a range of these items to ensure you get all the different elements that make up vitamin K.

Can supplements help Osteoarthritis?
The effects of seven supplements on OA (collagen hydrolysate, passion fruit peel extract, Curcuma longa extract, Boswellia serrata extract, curcumin, pycnogenol and L-carnitine) were reviewed in a meta-analysis and found to be associated with reduction of pain in the short term (Liu, Machado, Eyles, et al., 2018). However, much of this data was obtained through commercially sponsored small trials, the evidence is weak and long-term safety profiles are not known.
Chondroitin
Chondroitin is a supplement that is thought to stop the degradation of cartilage and help restore lost cartilage. It contains amino acids that contain sulphur, which are essential building blocks for cartilage (Singh, Noorbaloochi, MacDonald, et al., 2015).
Glucosamine
Glucosamine is available as a supplement and can be found naturally in the body, used as one of the building blocks of cartilage. It is available alone or in combination with other supplements such as chondroitin. The usual dose of glucosamine recommended on packages is 1500 mg per day.
A Cochrane review analysed 43 randomised controlled trials, totalling over 9000 people looking at the effects of the supplements chondroitin and glucosamine (Singh, Noorbaloochi, MacDonald, et al., 2015). While there were differences between the trials, reduced pain scores were seen in those people randomised to take chondroitin alone or in combination with glucosamine (Singh, Noorbaloochi, MacDonald, et al., 2015). A lesser effect was found in the meta-analysis by Lui et al, (Liu, Machado, Eyles, et al., 2018). More research is needed to understand the role of chondroitin and glucosamine in osteoarthritis and if there is any long-term benefit. However, the combination of low risk of side effects, and association with some reduction of pain means that it might be worth trying to see if it helps you.
Methylsulfonylmethane
Methylsulfonylmethane (MSM) is a sulphur based chemical that is found in some raw fruit and vegetables. There is some limited evidence to support the addition of MSM together with glucosamine and chondroitin (Lubis, Siagian, Wonggokusuma, et al., 2017).
Curcumin
Curcumin is the active ingredient in the spice turmeric and it makes up only 3% of the turmeric plant. Meta-analysis has found that curcumin (approximately 1000mg/day) can reduce arthritis associated pain and provide some functional benefit (W, YangMini, ParkSunmin, 2016). The long-term benefits of curcumin are still unknown, and more research is needed to answer this question. These studies have used supplements of curcumin in order to obtain clinically relevant effects. Since curcumin make up such a tiny percentage of turmeric, adding turmeric to cooking or taking a shot of turmeric is unlikely to provide you with enough curcumin to have any measurable effect. For example, if you take a turmeric shot, with 5g of turmeric, this would equate to approximately 150mg of curcumin. Therefore, in order to get a therapeutic level (500-1000mg), you would need to drink between 5-9 shots per day.

What role does diet play in rheumatoid arthritis?
Immune dysregulation plays an important role in the formation of autoimmune diseases. More evidence is emerging that dietary triggers and gut inflammation may play a role in generating this process (Alwarith, Kahleova, Rembert, et al., 2019).
Mediterranean Diet
A ‘Western” type diet can be broadly summarised as one consisting of high energy foods, refined carbohydrates (including sugar), high fat (particularly saturated fat), an unbalanced ratio of omega 3 and 6, low fibre and antioxidants, associated with increased chronic inflammation. While the Mediterranean diet, broadly summarised by a plant based diet, omega 3 fatty acids, rich in fruit, vegetables, extra-virgin olive oil and low in red meat and dairy has been found to be beneficial in RA (Philippou & Nikiphorou, 2018). Antioxidants are found primarily in fruit and vegetables, a key component of the Mediterranean diet.
Antioxidants
Antioxidants might both reduce the risk of formation of RA by decreasing inflammation, but also directly through their role in insulin resistance and obesity, both of which are risk factors for RA (Philippou & Nikiphorou, 2018). Omega 3 fatty acids, are also associated with a reduced risk of RA, possibly due to their anti-inflammatory properties (Gioxari, Kaliora, Marantidou, et al., 2018), with even some evidence that supplementation might delay the need for medications (Petersson, Philippou, Rodomar, et al., 2018).
Eating a Mediterranean style diet, therefore has the potential to not only reduce inflammation, but also help maintain a healthy weight (Philippou & Nikiphorou, 2018). Excessive body weight may also play a role not just in the likelihood of disease remission, but also severity (Alwarith, Kahleova, Rembert, et al., 2019).
Several studies have now shown an improvement in the symptoms of RA with plant based diets (Alwarith, Kahleova, Rembert, et al., 2019). One of the benefits of a plant based diet is the associated high fibre, which can also improve gut bacteria diversity and composition, so important in inflammation (Alwarith, Kahleova, Rembert, et al., 2019).
Vegan Diets
Although some of the trigger foods in RA patients are individualised, a vegan diet may help improve symptoms by eliminating many of these foods (Alwarith, Kahleova, Rembert, et al., 2019). While further research is needed, if you are suffering from RA, it might be worth trialling a vegan or Mediterranean diet as while they might benefit your RA, they are also good for general long-term health.
Can Supplements help Rheumatoid Arthritis?
Omega 3 Fatty Acids
Omega 3 supplements have been found to benefit the clinical outcome of RA (Akbar, Yang, Kurian, et al., 2017) and as mentioned above, may even delay the need for medications (Petersson, Philippou, Rodomar, et al., 2018). There is also limited evidence that omega 3 supplementation may benefit people with other types of autoimmune arthropathies such as systemic lupus erythematosus (SLE), but more research is needed (Akbar, Yang, Kurian, et al., 2017).
Probiotics
As the importance of gut health is now well recognised in inflammation, studies have tried to answer if probiotics can reduce inflammation and improve RA. In a meta-analysis of 9 studies, totalling 361 patients no improvement in RA was seen with probiotics (Mohammed, Khattab, Ahmed, et al., 2017). Instead try optimising your gut health with a range of fruit and vegetables, wholegrains and fermented food.
Vitamin D
Studies have found that people with RA have an increased likelihood of insufficient vitamin D, effects of supplementation on RA disease activity and symptoms are mixed (Guan, Hao, Guan, et al., 2020). Current recommendations are to maintain vitamin D at sufficient levels for general health.
Recommendations:
If you have RA aim for a plant based Mediterranean style diet:
- Include more extra virgin olive oil, rapeseed oil, avocado, seeds, nuts
- Eat at least 5 portions of fruit and vegetables a day.
- Replace refined carbohydrates (white bread, white rice) with whole grains (brown rice, brown bread, millet, bulgur wheat).
- Make Friday and Tuesday ‘fish’ night, where you and the family can enjoy a meal with oily fish. Or make yourself a big salad with mackerel. You can used tinned, smoked or some fresh from your fishmongers.Consider taking an omega 3 supplement (with EPA and DHA) especially if you do not eat oily fish
- Consider taking an omega 3 supplement (with EPA and DHA) especially if you do not eat oily fish
- Have at least 4 portions of unsalted nuts, seeds and legumes (like beans, lentils and chickpeas) each week.
- Remove convenience products that have high amounts of sugar and salt. And remove hidden sources of sugar(https://www.nhs.uk/live-well/eat-well/top-sources-of-added-sugar/).
- Regularly enjoy fermented food such as kimchi, sauerkraut, and kefir
- Aim to have sufficient levels of vitamin D, using supplements during autumn and winter months for general health
Consider the same diet as for RA if you have OA, but also consider taking a supplement such as curcumin, or chondroitin and glucosamine, to see if they help your pain.
Article Credit:
Dr Harriet Holme (https://healthyeatingdr.com/)
References
Akbar, U., Yang, M., Kurian, D. & Mohan, C. (2017) Omega-3 Fatty Acids in Rheumatic Diseases: A Critical Review. Journal of clinical rheumatology : practical reports on rheumatic & musculoskeletal diseases. 23 (6), 330–339.
Alwarith, J., Kahleova, H., Rembert, E., Yonas, W., et al. (2019) Nutrition Interventions in Rheumatoid Arthritis: The Potential Use of Plant-Based Diets. A Review. Frontiers in nutrition. 6141.
Chin, K.-Y. (2020) The Relationship between Vitamin K and Osteoarthritis: A Review of Current Evidence. Nutrients. 12 (5), 1208.
Gioxari, A., Kaliora, A.C., Marantidou, F. & Panagiotakos, D.P. (2018) Intake of ω-3 polyunsaturated fatty acids in patients with rheumatoid arthritis: A systematic review and meta-analysis. Nutrition. 45114–124.e114.
Guan, Y., Hao, Y., Guan, Y., Bu, H., et al. (2020) The Effect of Vitamin D Supplementation on Rheumatoid Arthritis Patients: A Systematic Review and Meta-Analysis. Frontiers in medicine. 7596007.
Kaliannan, K., Wang, B., Li, X.-Y., Kim, K.-J., et al. (2015) A host-microbiome interaction mediates the opposing effects of omega-6 and omega-3 fatty acids on metabolic endotoxemia. Scientific reports. 5 (1), 11276–17.
Liu, X., Machado, G.C., Eyles, J.P., Ravi, V., et al. (2018) Dietary supplements for treating osteoarthritis: a systematic review and meta-analysis. British Journal of Sports Medicine. 52 (3), 167–175.
Lu, B., Driban, J.B., Xu, C., Lapane, K.L., et al. (2017) Dietary Fat Intake and Radiographic Progression of Knee Osteoarthritis: Data From the Osteoarthritis Initiative. Arthritis care & research. 69 (3), 368–375.
Lubis, A.M.T., Siagian, C., Wonggokusuma, E., Marsetyo, A.F., et al. (2017) Comparison of Glucosamine-Chondroitin Sulfate with and without Methylsulfonylmethane in Grade I-II Knee Osteoarthritis: A Double Blind Randomized Controlled Trial. Acta medica Indonesiana. 49 (2), 105–111.
Mohammed, A.T., Khattab, M., Ahmed, A.M., Turk, T., et al. (2017) The therapeutic effect of probiotics on rheumatoid arthritis: a systematic review and meta-analysis of randomized control trials. Clinical rheumatology. 36 (12), 2697–2707.
Petersson, S., Philippou, E., Rodomar, C. & Nikiphorou, E. (2018) The Mediterranean diet, fish oil supplements and Rheumatoid arthritis outcomes: evidence from clinical trials. Autoimmunity reviews. 17 (11), 1105–1114.
Philippou, E. & Nikiphorou, E. (2018) Are we really what we eat? Nutrition and its role in the onset of rheumatoid arthritis. Autoimmunity reviews. 17 (11), 1074–1077.
Schett, G., Kleyer, A., Perricone, C., Sahinbegovic, E., et al. (2013) Diabetes is an independent predictor for severe osteoarthritis: results from a longitudinal cohort study. Diabetes care. 36 (2), 403–409.
Singh, J.A., Noorbaloochi, S., MacDonald, R. & Maxwell, L.J. (2015) Chondroitin for osteoarthritis. Jasvinder A Singh (ed.). The Cochrane database of systematic reviews. 1 (5), CD005614.
Thomas, S., Browne, H., Mobasheri, A. & Rayman, M.P. (2018) What is the evidence for a role for diet and nutrition in osteoarthritis? Rheumatology (Oxford, England). 57 (suppl_4), iv61–iv74.
Uthman, O.A., van der Windt, D.A., Jordan, J.L., Dziedzic, K.S., et al. (2013) Exercise for lower limb osteoarthritis: systematic review incorporating trial sequential analysis and network meta-analysis. BMJ (Clinical research ed.). 347 (sep20 1).
Zhuo, Q., Yang, W., Chen, J. & Wang, Y. (2012) Metabolic syndrome meets osteoarthritis. Nature reviews. Rheumatology. 8 (12), 729–737.
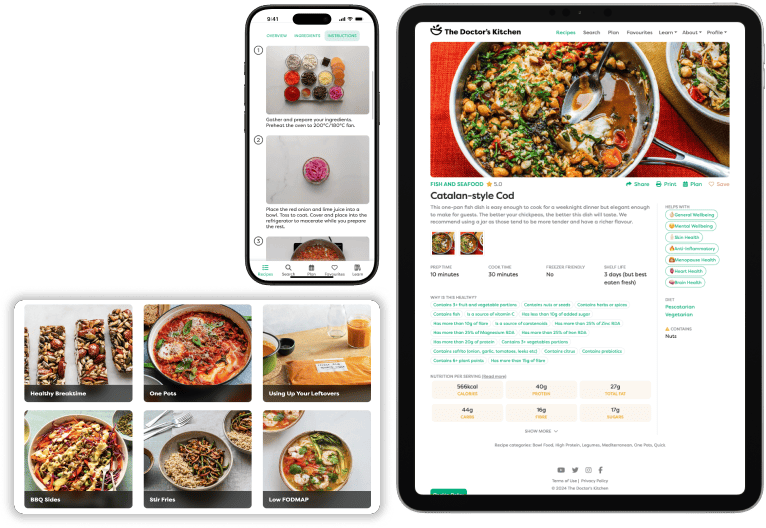
- Access over 800 research backed recipes
- Personalise food for your unique health needs