


17 Apr 2024
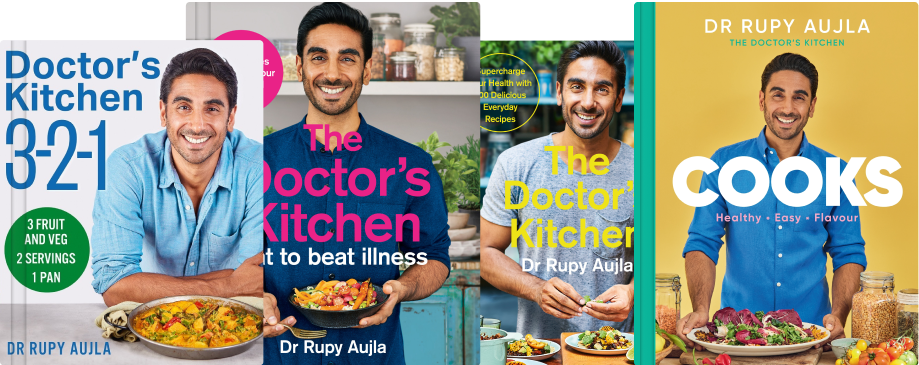
Our cookbooks are a culinary journey through food in medicine


11 Apr 2024

09 Apr 2024

05 Apr 2024

28 Mar 2024

22 Mar 2024

15 Mar 2024

29 Feb 2024

22 Feb 2024

16 Feb 2024

14 Feb 2024

08 Feb 2024

02 Feb 2024
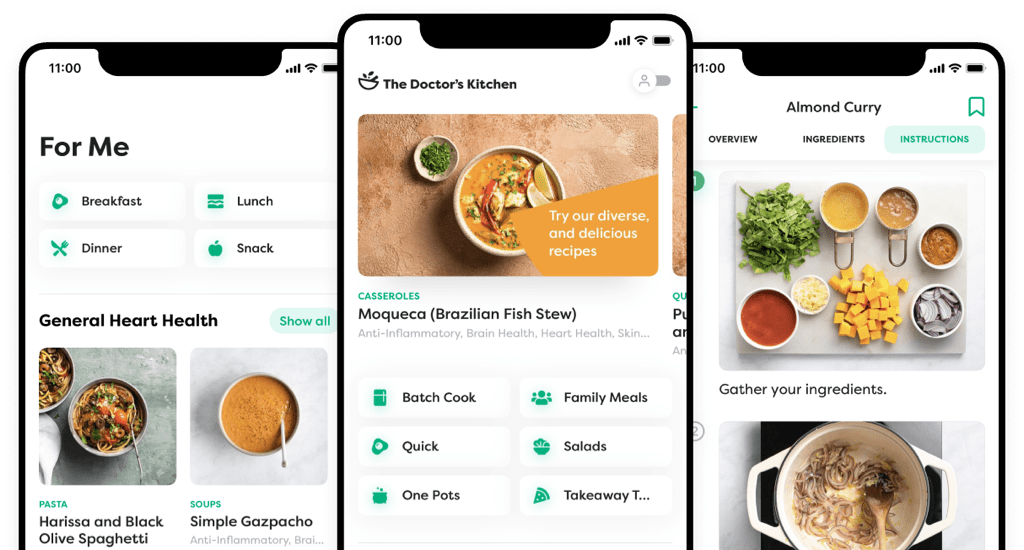
Download our app to get access to all of our recipes, with specific suggestions tailored to your health needs.


Sign up to our newsletter and receive a free copy of our breakfast, lunch and dinner plan to kick start your healthy eating.